Leading third-party administrator for employers who self-fund their health care benefits.
At Pinnacle, we simplify health benefits administration for self-funded employers. These solutions include personalized plan designs, concierge services, navigation technology, competitive network solutions, innovative cost management programs, integrated disease management and wellness options, and analytics and insights that fit your needs and budget, big and small.
Leading third-party administrator for employers who self-fund their health care benefits.
At Pinnacle, we simplify health benefits administration for self-funded employers. These solutions include personalized plan designs, concierge services, navigation technology, competitive network solutions, innovative cost management programs, integrated disease management and wellness options, and analytics and insights that fit your needs and budget, big and small.
Pinnacle Mission
Pinnacle’s mission is to offer custom health benefits solutions to fit your client’s needs. Pinnacle achieves this mission by providing a holistic approach to supporting our members in need, managing our clients’ health plan by becoming an extension of their HR Team, and partnering with our broker partners to manage our clients’ best-in-class benefits.
- Independently Owned
- Full service TPA providing concierge service to self-insured groups
- 96% client retention
- Experience serving a broad and diverse client base
- 30+ years providing TPA Services
- Flexible build to suit administration on Pinnacle owned and supported systems
- National capability with robust network partners
- Claims and cost management professionals
Custom Health Benefit Solutions
Holistic approach to supporting members needs
Experts at managing health plan by becoming an extension of HR Team
Partner with brokers to manage best-in-class benefits for clients
Our One-Stop-Shop Solutions
Benefit Administration
- Medical Plan Administration
- Dental Plan Administration
- Vision Plan Administration
- Stop-Loss Quotes and Administration
- HRA/FSA/HSA
- Spousal HRA
- COBRA
- Pharmacy Benefit Management
Health Management
- Pinnacle Health Management Essentials
- Pinnacle Health Management Prevention Plus
- Pinnacle Health Management Advocate Plus
Other Services
- Provider Contracting
- Managing Services Organization (MSO)
- Rightway Mobile App
- Consolidated Billing and Eligibility
Hospital Support
At Pinnacle, we offer custom health benefit solutions that help your hospital support the people who make a difference every day.
- Employee Focus: We develop strategies that address common labor issues and support employee well-being.
- Domestic Utilization: Our proven approach enhances utilization across your facilities and with your providers.
- Flexibility: Our solutions offer flexible financial arrangements seamlessly integrated with your existing systems.
- Expertise: With decades of experience in healthcare and clinic management, our team is uniquely equipped to design tailored solutions that meet your specific needs and objectives.
- Independence: As an independently owned TPA, we operate free from provider partnership conflicts, ensuring our sole focus is on delivering what's best for you.


PinnacleRx Solutions
Navigating the complexities of the ever-changing pharmacy marketplace is what we do. At PinnacleRx Solutions, we take a consultative approach to fulfilling pharmacy benefit needs.
- Custom Plan Designs
- Broad Formulary
- Health Management
- Independently Owned
- Transparency & Visibility
- Monitoring & Reporting
Pinnacle Health Management Process
Pinnacle’s Health Management program provides personalized care management and wellness services to your clients and their families. Our team consists of Registered Nurses, Care Coordinators, and Licensed Behavioral Therapists. They support and advocate wellness, prevention of uncontrolled disease states and the provision of the highest quality care by improving ease of access and targeting the most appropriate levels of care.
Pinnacle is unique in that we can integrate our programs with your vendors. We can also customize our programs to offer incentives for employee participation in conjunction with our health management and wellness programs.
We’re also effective in utilization management, discharge planning, clinical case appeals, provider certification, and quality of care associated with each facility to ensure that the least costly, yet most effective, treatment is used.
The goal of our health management program is to assist participants in managing their chronic health conditions, improving health outcomes, and preventing related risks and complications.
Health Management Programs
Pinnacle Health Management
Essentials
-
Chronic Disease Management (nurse calls included)
-
Asthma
-
Diabetes
-
Hypertension/ High Blood Pressure
-
Hyperlipidemia/ High Cholesterol
Pinnacle Health Management
Prevention Plus
-
Includes Pinnacle Health Management Essentials
-
Prevention Programs
-
Uplift
-
Mom-to-Be
-
Nicotine Cessation
-
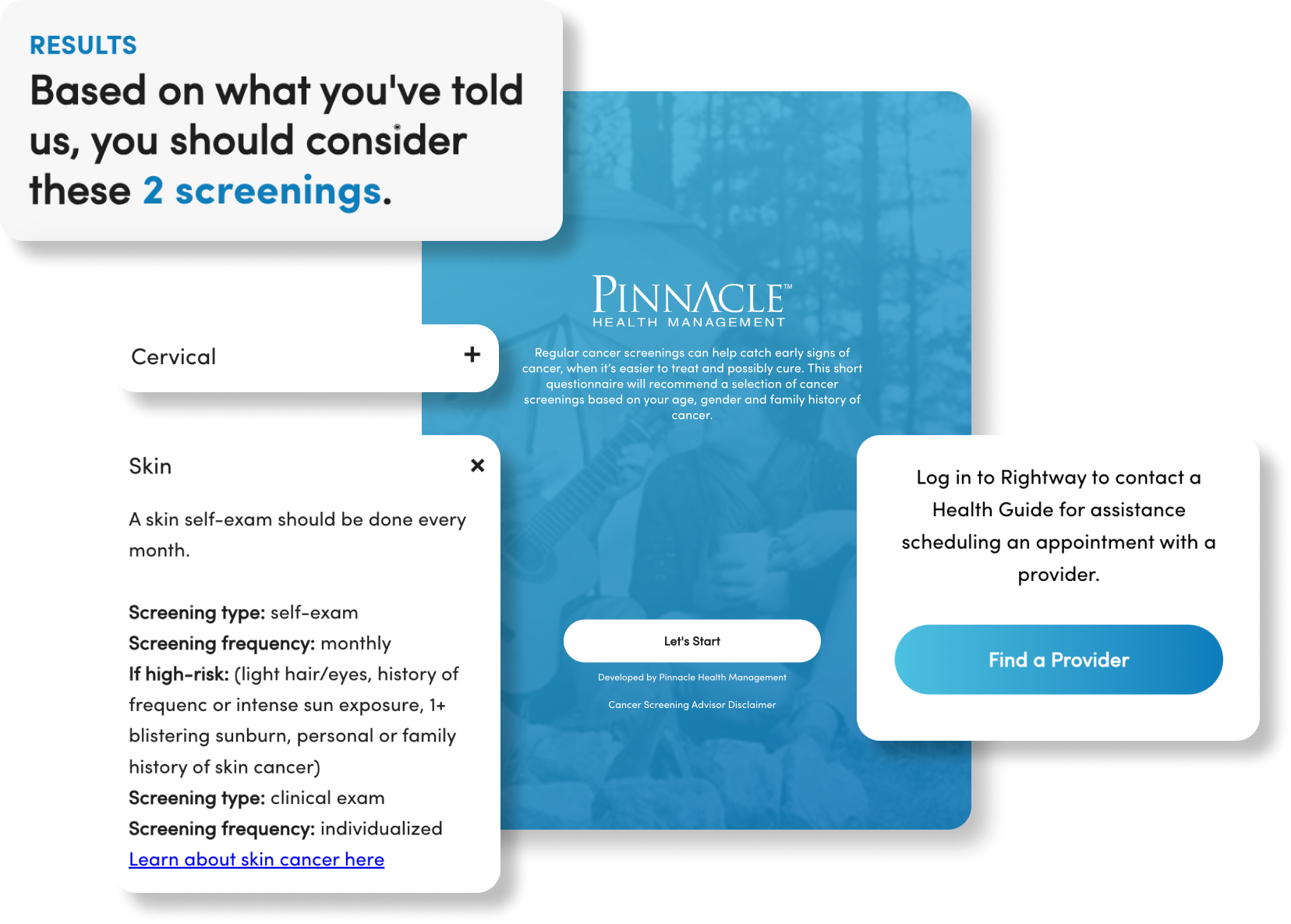
Cancer Screening
-
Wellness Engagement
-
Quarterly Newsletters
-
Monthly Toolkits
-
Monthly Webinars
Pinnacle Health Management
Advocate Plus
-
Includes Pinnacle Health Management Prevention Plus
-
Wellness Coaching & Challenges
-
Customized Quarterly Challenges
-
Group Wellness Coaching
-
Nutritionist Coaching
-
Rightware Care Navigation & Concierge
-
Clinical Guidance
-
Benefits Navigation
-
Bill Advocacy
-
Provider Search
Pinnacle Health Management
Additional Services
-
Biometric Testing
-
Health Risk Assessments
-
Predictive Modeling
-
Flu Shots
-
Covid-19 Testing
Online Tools
Whether you’re an employer, plan participant, broker, or provider, you have secure access to our proprietary technology and online tools to retrieve health benefit information. Our online tools allow access to reports, updates to profile information, eligibility and enrollment, and secure payments.
-
Pinnacle Employee Resource Center (PERC)
-
Healthview Employee Resource
-
Online Provider Information Service (OPIS)
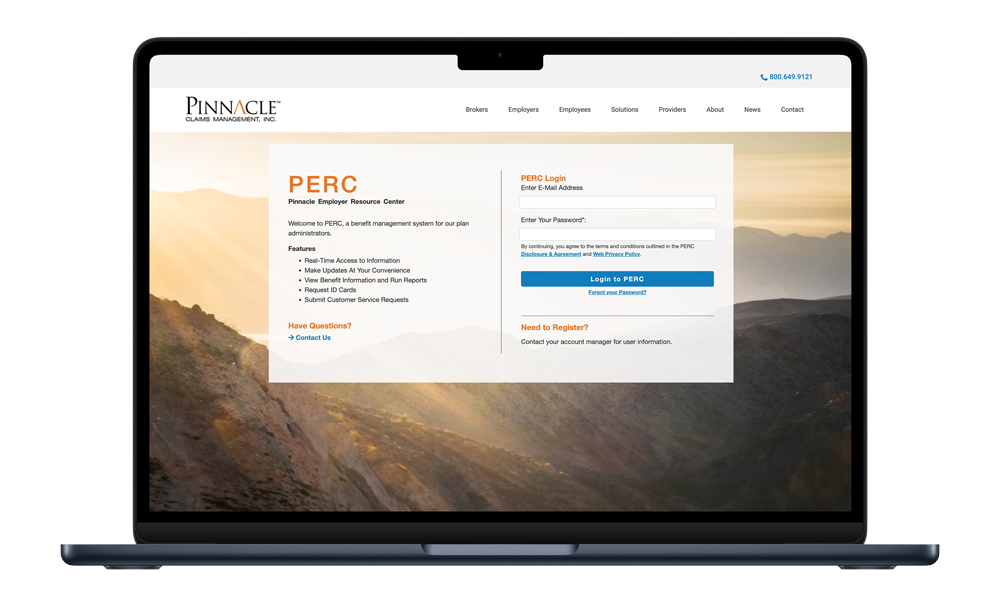
Pinnacle Employee Resource Center (PERC)
PERC is a free tool available to our brokers and employers to easily access and update their health benefits information. We offer one-on-one program training so you can begin accessing your plan information immediately and understand how to maximize all that this resource has to offer.
Driven by the specific needs of our brokers and employers, our proprietary online health benefits tool can be customized to provide access to the information and reports you need most.
Healthview Employee Resource
We help make managing your employee benefits a little easier by giving your employees convenient access to their health benefits information via a secure, easy-to-use online tool. HealthView is a free tool available 24 hours a day, seven days a week. Empower your employees to stay in control of their health benefits with this online tool.
Online Provider Information Service (OPIS)
OPIS allows health care providers direct access to patient information via this convenient online tool. Providers can look up eligibility, deductibles, claim status, benefit plan information and more so that they do not have to call customer service to obtain such information.
OPIS is offered to providers free of charge and is available 24 hours a day, seven days a week through our interactive intelligence phone system (IVR).
Rightway App
Pinnacle also partners with Rightway to provide concierge member engagement via our app and expert health guides. Rightway provides member engagement via app and expert health guides.
- Single point of contact care advocate assigned to each member
- Health Guides steer members to the top
in-network providers. - Scheduling provider appointments
- Benefits tracking and explanations
- Billing support
- Gaps in care outreach
- Referrals to other employer programs
Rightway App
Pinnacle also partners with Rightway to provide concierge member engagement via our app and expert health guides. Rightway provides member engagement via app and expert health guides.
- Single point of contact care advocate assigned to each member
- Health Guides steer members to the top
in-network providers. - Scheduling provider appointments
- Benefits tracking and explanations
- Billing support
- Gaps in care outreach
- Referrals to other employer programs

Pinnacle Concierge Service
Pinnacle’s core value is to provide concierge service to our members through our dedicated operations teams: account management, customer service, claims excellence, legal and compliance, and implementation.
-
Account Management Structure
-
Exceptional Customer Service
-
Claims Excellence
-
Legal & Compliance
-
Implementation

Account Management Structure
Dedicated Account Management Teams
- Led by senior director, account management and senior account manager/account manager supported by client service representative
- 10 years average tenure
- Virtual/onsite OE presentations and support
- Routine scheduled on-site service visits to address health plan
- Annual in-depth review of claims data and health trends

Exceptional Customer Service
- Dedicated customer service team
- Extensive training on client culture and health plan before go live
- Care navigation and holistic member approach
- Bilingual customer service representatives
- Ops metrics
- First Call Resolution - 88.11%
- Average Speed of Answer - 00:27
- Service Level (SLA) - 81.77% of calls answered within 30 seconds or less
- Abandonment Rate - 0.82%

Claims Excellence
- Average Turnaround Time: 6.86 Days
- 52% of claims processed in 1 day
- 55% auto adjudication rate
- Claims processing accuracy:
- Procedural Accuracy – 96.61%
- Financial Accuracy – 99.05%

Legal & Compliance
- In-house ERISA attorneys
- Expertise in corporate and plan governance
- Summary Plan Description
– Review, development & distribution - Summary of Benefits & Coverage
– Bilingual availability - Government required filings
- Legislative coverage notices
- Subrogation
- ACA reporting tool
- Compliant with Consolidated Appropriations Act & Transparency In Coverage Regulations

Implementation
Experience Transition Management Team
- Experienced installation staff supported by SMEs and system quality controls
- Transition issues supported by Pinnacle team prior to go-live date
Customized Implementation Timeline
- Implementations require 90-120 days
- Weekly implementation meetings with broker and client
- Project managers assigned to each implementation
- Project status/risk management/decision logs provide transparency
- Each task tracked and assigned to ensure accountability
Springbuk
Pinnacle offers comprehensive reporting to provide direct oversight to help you take control of your health care dollars. Our state of the art reporting solutions, allow health benefit managers and brokers to conduct health trend analysis from an easy-to-use, web-based platform. We work with you to tailor programs that maximize appropriate utilization and generate the most cost-effective benefit solutions.
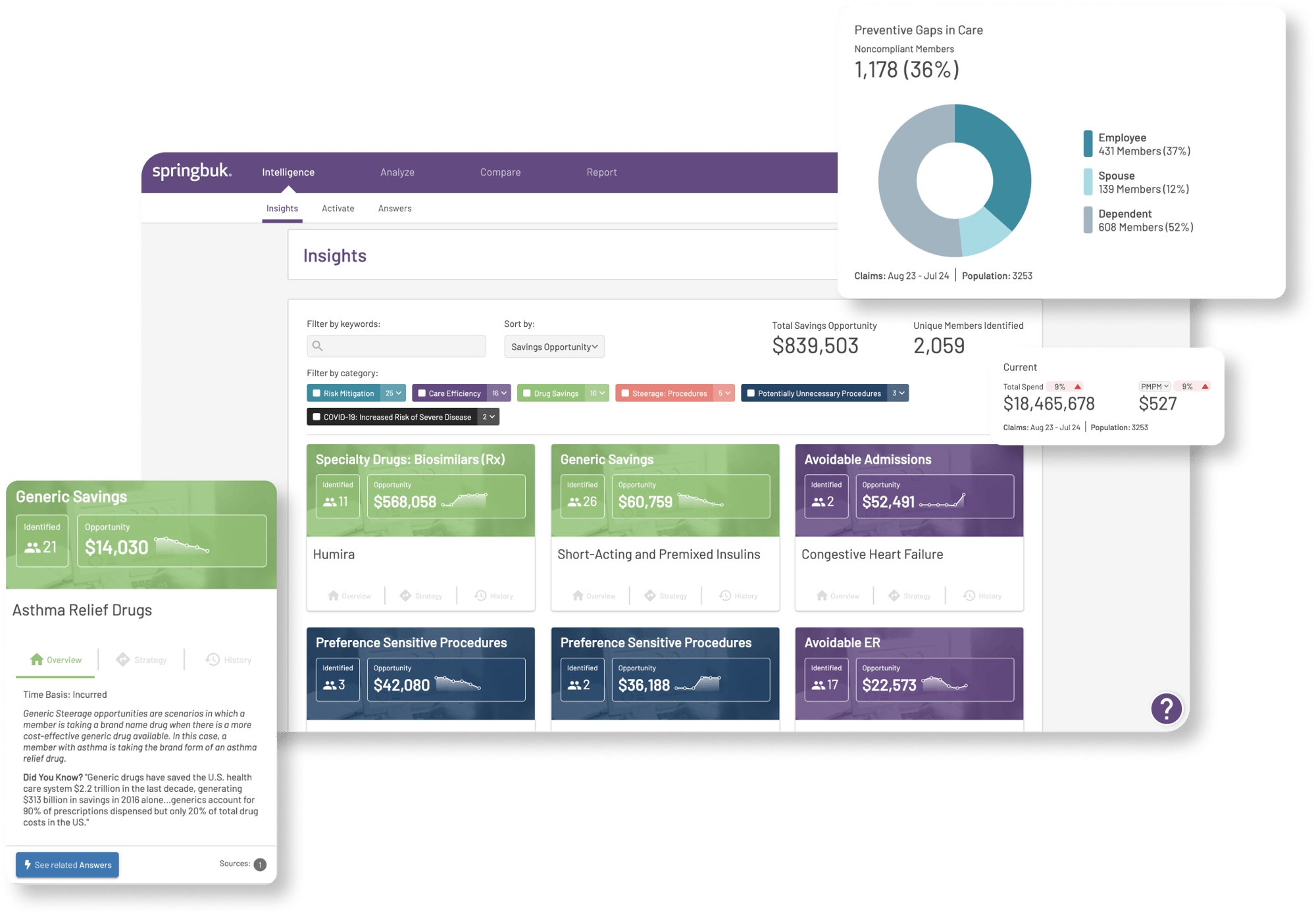
A World of Insight at Your Fingertips
- A high-level view of your population
- Identify and understand population trends
- Quickly analyze chronic conditions
- Track events to clearly identify value
- Reporting made simple
- Flexible and customizable data visualization
- Curated insights for actionable opportunities
- Answer your questions instantly
Complex Group
Plan Details
- 6 Medical Plans (3 Pinnacle, 3 Kaiser) for Active, Retiree and Out of State
- 1 Dental Plan (Delta) - Eligibility services
- 1 Vision Plan (VSP) - Eligibility services
- 1 Pharmacy Plan (Magellan)
Networks
- 1 Medical (Anthem PPO)
- 1 Dental (Delta) - Eligibility services
- 1 Vision (VSP) - Eligibility services
- 1 Pharmacy (Magellan) - not sending Kaiser pharmacy or Medicare Supplement pharmacy data.
Products Pinnacle is Administering
- Third Party PCMI Administration
- Eligibility Administration (Rx, Dental, Vision)
- COBRA Administration
- Retiree Administration
- Network Administration
- Telehealth
- Nurseline
- Stop Loss Administration
- Compliance Documents
- Consolidated Billing Services
Operation Metrics
Member Calls
- First call resolution: 88.11%
- Average speed of answer: 0:27
- Service Level (SLA): 81.77% of calls answered within 30 seconds or less
- Abandonment rate: 0.82%
Claims
- Average turnaround time: 3.2 days
- Claims accuracy
- Procedural: 98.6%
- Financial: 99.1%
What Pinnacle Offers
- Price transparency and competitive overall cost
- Breadth of service offering
- Flexibility and customization
- Network access
- Reputation and financial stability
- Operational excellence
- Implementation and integration capabilities
- Technology and platform
- User experience and customer support
- Reporting and analytics
- Innovative solutions
- Low employee disruption and HR workload
- Compliance expertise
We care about our brokers and their clients so they can focus on their most valuable resource—their people.
Contact Us
Have any questions about self-funding, customizing your healthcare packages or administration benefits, or need additional support? Contact us today.
Learn More
Want to learn more about Pinnacle Claims Management, Inc? Visit our website pinnacletpa.com.
Request for Proposal
Request an RFP to explore how Pinnacle Claims Management can support your growth and deliver excellence for your clients.
2026 Copyright © Pinnacle Claims Management Inc. | Privacy Policy and Terms of Use